Leg Swelling and Leg Pain
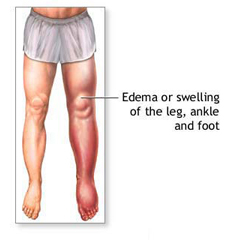 Leg swelling occurs as the varicose vein and the vein valves become more abnormal. The poorly functioning valves allow blood to flow backward, which causes pooling in the veins. Symptoms can include: aching, cramping, tired legs, swelling, heaviness, restless legs, and itching. The pooling causes increased pressure inside the veins. This increased pressure causes the veins to distend and become “leaky,” allowing fluid inside the veins to leak outside the vein into surrounding tissue causing swelling. The swelling can cause the legs to ache and feel heavy. Leg pain is caused not only from the effects of swelling, but also from the effects of congestion or pooling in the muscles. The discomfort of both leg swelling and leg pain can be improved with compression stockings or possibly treated with endovenous laser ablation.
Leg swelling occurs as the varicose vein and the vein valves become more abnormal. The poorly functioning valves allow blood to flow backward, which causes pooling in the veins. Symptoms can include: aching, cramping, tired legs, swelling, heaviness, restless legs, and itching. The pooling causes increased pressure inside the veins. This increased pressure causes the veins to distend and become “leaky,” allowing fluid inside the veins to leak outside the vein into surrounding tissue causing swelling. The swelling can cause the legs to ache and feel heavy. Leg pain is caused not only from the effects of swelling, but also from the effects of congestion or pooling in the muscles. The discomfort of both leg swelling and leg pain can be improved with compression stockings or possibly treated with endovenous laser ablation.
Chronic Venous Insufficiency
When venous disease is long standing, it can become chronic venous insufficiency (CVI). CVI occurs from chronic pooling and congestion caused by leaky varicose veins, from chronic obstruction in veins due to repeated clots (thrombosis), or from repeated inflammation of the veins (phlebitis). As this condition worsens and become severe, skin changes and leg ulcerations can occur. Treatment is aimed at relieving the swelling in the legs. This can be achieved with compression stockings or with endovenous laser ablation.
Leg Skin Changes
 The skin changes associated with chronic venous insufficiency are sometimes called venous stasis dermatitis and are the result of long-standing swelling and increased pressure in the veins.
The skin changes associated with chronic venous insufficiency are sometimes called venous stasis dermatitis and are the result of long-standing swelling and increased pressure in the veins.
Eventually the constant swelling, decreased blood flow to the area, and increased pressure result in decreased movement of oxygen and nutrients to the skin. The tissue becomes damaged and the skin becomes inflamed (cellulitis). The skin eventually becomes reddish brown, hard, thick, leathery dry, and itchy.
Although treatment will probably not reverse the skin changes, treatment aimed at relieving the swelling and decreasing the pressure in the veins will improve symptoms and prevent progressions to skin ulcerations. Treatments aimed at reducing the swelling may involve a combination of treatments such as prescription drugs, compression stockings, and endovenous laser ablation.
Leg Ulcers
 When venous disease and blood pooling becomes severe, venous stasis ulcers can occur in the skin. These ulcers usually occur around the ankles and are thought to be caused from long-standing “water logging” or pooling from blood congestion in the affected leg.
When venous disease and blood pooling becomes severe, venous stasis ulcers can occur in the skin. These ulcers usually occur around the ankles and are thought to be caused from long-standing “water logging” or pooling from blood congestion in the affected leg.
Long standing congestion is suspected to cause obstruction in the blood flow, which then causes changes in the skin pressure. These changes cause the oxygen levels in that area to become decreased. With the blood flow obstruction and the decreased oxygen levels, skin ulcers begin to form. These venous ulcers can be painful, and treatment can be lengthy and frustrating.
In many cases, if a varicose vein is diagnosed and considered a cause for the venous ulcer, treating the varicose vein with endovenous laser ablation will help redirect the blood flow, relieve the venous congestion, and improve the leg ulcer.
Phlebitis
Phlebitis means inflammation of the vein. It can affect the superficial veins or the deep veins. Thrombus means clot. Because thrombus is almost always associated with phlebitis, some doctors use the terms thrombosis, phlebitis, and thrombophlebitis interchangeably. If a clot is in a vein, it causes stretching and inflammation of the vein. If a clot is in one of the superficial veins it is called superficial thrombophlebitis and if a clot is in one of the deep veins it is called deep vein thrombosis (DVT).
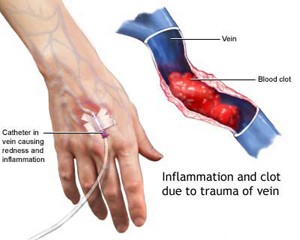 Superficial thrombophlebitis (ST) often develops in a varicose vein where the blood flow has become sluggish. Although ST does occur in people who have varicose veins, most people with varicose veins do not develop ST. ST can also occur after surgery, injury, intense exercise, in response to a medical or surgical disease, or from genetic blood clotting disorders. The symptoms include a tender, cord-like vein that is sensitive to pressure, redness, and warmth in the area from the inflammation and swelling around the affected vein.
Superficial thrombophlebitis (ST) often develops in a varicose vein where the blood flow has become sluggish. Although ST does occur in people who have varicose veins, most people with varicose veins do not develop ST. ST can also occur after surgery, injury, intense exercise, in response to a medical or surgical disease, or from genetic blood clotting disorders. The symptoms include a tender, cord-like vein that is sensitive to pressure, redness, and warmth in the area from the inflammation and swelling around the affected vein.
Even a slight injury can cause a varicose vein to become inflamed. This sudden (acute) inflammation causes a small clot to adhere to the vein wall. Unlike deep veins, the superficial veins do not have surrounding muscles to squeeze and dislodge the clot (thrombus). For this reason, ST rarely causes an embolism, a sometimes serious condition when the clot is dislodged to other parts of the body.
An ultrasound may be able to detect a clot in the vein. Treatment may include taking anti-inflammatory drugs such as aspirin or ibuprofen; warm, moist compresses to the area (be careful to avoid burning the skin); and elevation of the leg. Occasionally the clot may be removed and compression stockings are worn. With proper treatment, ST usually resolves in one to two weeks. If you have varicose veins that predisposed you to ST, treating the varicose vein with endovenous ablation can help prevent recurrent ST.
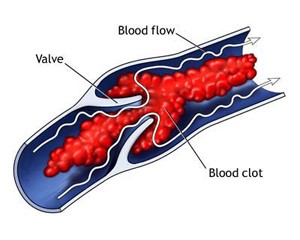 Deep vein thrombosis (DVT)occurs when a clot develops in a deep vein. Unlike ST, in deep veins little inflammation occurs with the clot formation. Therefore, the clot is less likely to adhere to the vein wall and more likely to break loose, travel downstream, become lodged in an artery, and block blood flow (an embolus) – which is a serious condition. In addition, deep veins are surrounded by muscles. The squeezing action of the muscle can cause the clot to break loose and become an embolus. Therefore, DVT can be a potentially serious situation. Because blood from the legs drains directly into the heart and lungs, an embolus from the legs could become a pulmonary embolism.
Deep vein thrombosis (DVT)occurs when a clot develops in a deep vein. Unlike ST, in deep veins little inflammation occurs with the clot formation. Therefore, the clot is less likely to adhere to the vein wall and more likely to break loose, travel downstream, become lodged in an artery, and block blood flow (an embolus) – which is a serious condition. In addition, deep veins are surrounded by muscles. The squeezing action of the muscle can cause the clot to break loose and become an embolus. Therefore, DVT can be a potentially serious situation. Because blood from the legs drains directly into the heart and lungs, an embolus from the legs could become a pulmonary embolism.
There are many causes of DVT: injury to the vein (which may occur during surgery), decreased blood flow, or a genetic tendency to form clots, certain medical conditions, certain medications, dehydration, prolonged bedrest, prolonged sitting, smoking and more.
Because DVT usually causes little inflammation, pain and redness over the skin is usually minimal. 50% of the people with DVT have no symptoms at all. However, when the DVT blocks a large leg vein, swelling may occur in the foot, calf, leg or thigh, depending on where the blockage occurs. The area may become painful, tender to the touch and warm.
 DVT can be difficult for doctors to diagnose, however an ultrasound can frequently detect a clot. Treatment is aimed at preventing the clot from enlarging and from becoming an embolus. Occasionally people need to be hospitalized, but some can be treated at home. Swelling of the leg can be helped with bedrest, leg elevation and sometime compressions bandages. Medications to prevent clot formation and sometimes medications to dissolve the clot may also be used. In more complicated cases, filters may be placed inside the large veins to prevent the vein from dislodging to the heart or lungs.
DVT can be difficult for doctors to diagnose, however an ultrasound can frequently detect a clot. Treatment is aimed at preventing the clot from enlarging and from becoming an embolus. Occasionally people need to be hospitalized, but some can be treated at home. Swelling of the leg can be helped with bedrest, leg elevation and sometime compressions bandages. Medications to prevent clot formation and sometimes medications to dissolve the clot may also be used. In more complicated cases, filters may be placed inside the large veins to prevent the vein from dislodging to the heart or lungs.
Vascular Malformations
Most vascular malformations are genetic — meaning you are born with them. Although these lesions/conditions are present at birth, they may not be visible until weeks or even years after birth. While they sometimes seem to grow quite rapidly, their growth is usually gradual and steady during the first year of life.
There are several sub-types of vascular malformation: capillary malformations, venous malformations, lymphatic malformations, arteriovenous malformations, and combined malformations. The severity varies greatly both within and among each group. Also, because these malformations are made up of vessels, and blood flows through these vessels, they are sometimes categorized as either slow or fast flow.
Venous Malformations
Venous malformations (VM) are superficial or deep veins (or both) that are either abnormally formed or unusually dilated. VMs can be genetic or acquired. Although most VMs are always present at birth, they may not show up until years later. Some VMs may be acquired, but the causes are not well understood. VMs usually are slow growing and usually grow as the body grows. However, certain situations such as surgery, trauma, infection, hormonal changes (like puberty, pregnancy, menopause) may cause a more rapid growth. VMs are most common in the legs, but may be found in anywhere in the body.
There is a wide variation of VMs and their appearance depends on their location, whether they are superficial or deep and whether they are localized or diffuse. If they are located in the skin, they may be visible as maroonish-red to purplish-blue, depending on how deep they are. Usually the closer they are located to the skin, the darker the color. A deeper lesion may not show color and only reveal itself as a protruding mass.
The symptoms of VMs vary greatly. Most VMs are benign and never cause a problem. Depending on their nature, size and location others can be very problematic causing swelling and pain. Treatment also depends on the nature, size, and location. VMs close to the skin can be treated with sclerotherapy, cutaneous laser, or surgical excision.

